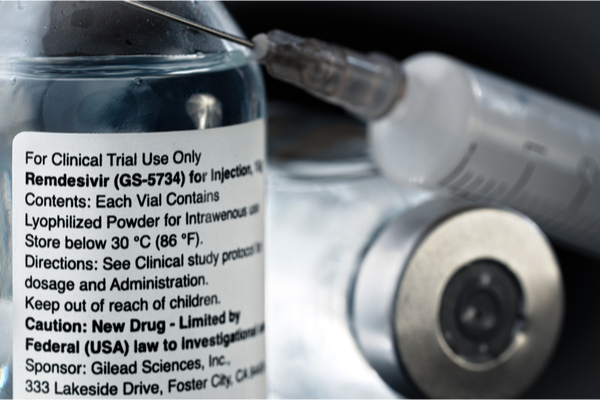
Could an antiviral drug originally developed to fight Ebola turn out to be an effective therapy in the fight against coronavirus? Two days after the release of promising clinical trials data on remdesivir, the US Food and Drug Administration granted emergency use of the drug for the treatment of adults and children who are hospitalized with severe COVID-19. The speedy authorization gives doctors an option for helping patients who have low blood oxygen levels or who need oxygen or mechanical ventilation.
Remdesivir, developed by California-based drugmaker Gilead Sciences Inc., appears to “block” COVID-19. In an interview with NBC News Today on April 29, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases (NIAID), said the drug “has a clear-cut, significant, positive effect in diminishing the time to recovery.” He revealed that in a large international study, patients who took remdesivir needed an average of 11 days to recover from COVID-19, compared to 15 days for those in the study who received a placebo. “Although a 31% improvement doesn’t seem like a knockout 100%, it is a very important proof of concept,” said Dr. Fauci. “What it has proven is that a drug can block this virus.”
Remdesivir is part of the World Health Organization’s “Solidarity” trial, which began in February. Dr. Fauci told NBC News Today that the “primary endpoint of the study was the patients’ time to recover, and specifically their “ability to be discharged” from the hospital. As well as a quicker recovery rate, the fatality rate was more favorable in the remdesivir group—8% of patients died, compared to 11% in the placebo group.
In an earlier study involving patients with severe cases of COVID-19 in hospitals in Hubei, China, the drug didn’t accelerate recovery or reduce deaths compared to a placebo. However, that study was stopped early because not enough people could be recruited as the epidemic tailed off in China. In a statement, Gilead said the termination of the trial didn’t mean it was a failure, simply that the results were inconclusive, reported Clinical Trials Arena. On April 29, a few hours after Dr. Fauci’s announcement, the full study from China was published in The Lancet.
More trials of remdesivir are ongoing, but in the meantime, the medical community has welcomed what appears to be a glimmer of hope for COVID-19 patients. “It’s an exciting development to have a therapy that may be the first approved treatment for COVID-19,” Ryan Steele, DO, an assistant professor of clinical medicine in rheumatology, allergy, and immunology at Yale School of Medicine, stated in a recent interview with Health magazine. “Although all the data has not been seen by the broader medical community yet, we are headed in the right direction.”
It will be some time before we know if remdesivir is a true game changer in the fight against COVID-19, Linda Anegawa, MD, an internist with virtual primary care platform PlushCare, said in an interview with Health magazine. She points out that the study lacks statistical significance—meaning there is a likelihood that these numbers came about just by chance, rather than by a true clinical effect.
“We will need a much larger study to be done in order to determine this,” says Dr. Anegawa. “Many patients in the study who participated didn’t seem to be all that ill, so they may have recovered naturally on their own regardless of whether they received the drug. In addition, we don’t know if the drug could have harmed patients or caused some of the adverse outcomes that were reported (such as kidney or liver failure). This is because the study lacked what is known as a control group—a group of similar patients who did not receive remdesivir, to compare with the treatment group.”
When the full, detailed data about the patients, how sick they were, and any potential side effects is released, it will be easier to evaluate the results of the trial. Hopefully, we shouldn’t have long to wait. In the NBC News Today interview, Dr. Fauci said this data is expected to be released within days. The FDA’s emergency use authorization isn’t the same as a drug approval. The authorization is temporary and may be revoked at any time. In a statement on the company’s website updated June 24, Gilead said it has been ramping up its production of the drug and expects to have more than 2 million courses of treatment by the end of 2020.
Gilead’s Chairman and CEO Daniel O’Day recently disclosed details of the drug’s pricing. In an open letter published June 29, O’Day said that private health insurers in the US would be charged $520 per vial of the intravenous drug, while the US government will pay $390 per dose. Based on a typical course of treatment, the total cost would be $3,120 for a privately insured patient and $2,340 for someone covered under a government program, such as Medicaid. What any one person might may pay out of pocket would depend on their insurance coverage and other variables, reports CBS News.
“The bottom line is, testing antiviral medications such as remdesivir is a great start to potentially investigating multiple different antivirals and antiviral combinations in the fight against COVID-19,” says Dr. Anegawa. “But there is still much that we don’t know, and this reinforces my belief that we are still far away from having a Tamiflu-like agent that could be made widely available to patients.”
Dr. Steele believes that as the months progress, remdesivir will be only one of a list of recommended and approved therapies for COVID-19. “This will be critical to handling current and future spikes of cases,” he says. “Ultimately, we need long-term strategies to continue to live and work while we try to develop a vaccine for widespread use.”
—
Photo Credit: Lubo Ivanko / Shutterstock.com