Heart attack, stroke, pulmonary embolism—all three medical emergencies happen in different parts of the body, and yet they have something in common: They can all be caused by a blood clot.
The National Blood Clot Alliance (NBCA) states that approximately one person dies every six minutes as a result of a blood clot. They’re so dangerous because they can impede or block blood flow to vital organs in the body. Not all blood clots are created equal, though. Blood clots “can range from mildly symptomatic and recoverable to fatal,” Elad I. Levy, MD, professor and chair of neurosurgery at the University at Buffalo, said in an interview with Health magazine.
What Exactly is a Blood Clot?
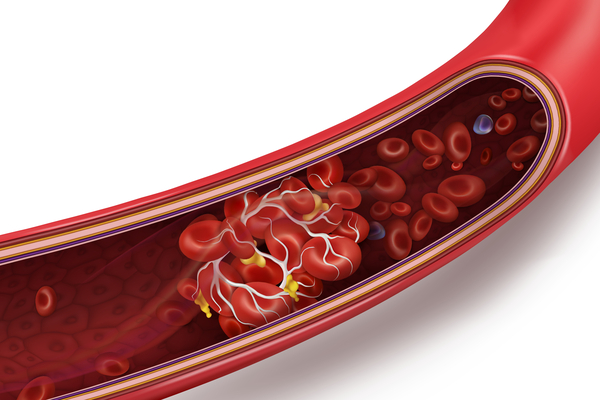
According to the Mayo Clinic, your blood is typically in a liquid state, but a blood clot is a gel-like clump of blood. Blood clots can be helpful in certain situations, like when you have an injury or a cut, to help plug the injured blood vessel and stop the bleeding. But blood clots can form inside your body without a good reason, and block blood vessels—this is called thrombosis. Those can travel to critical areas of your body, like your lungs, brain, or heart, causing serious and sometimes fatal complications like a pulmonary embolism (when a blood clot travels to your lungs), a stroke (when one reaches the brain), or a heart attack (a blood clot in the heart).
While your overall risk of having a blood clot is fairly low, they can and do happen. In order for blood to reach all parts of your body—from the top of your head to the tip of your toes—you have a circulatory system which is made up of blood vessels called veins and arteries. (Arteries carry oxygen-rich blood from the heart to other parts of the body; veins carry oxygen-poor blood back to the heart to get reoxygenated.)
The Two Types of Blood Clots and Their Symptoms
Because there are two types of vessels that carry blood throughout your body, there are also two types of blood clots: arterial clots, which occur in the arteries, and venous clots, which form in the veins. Blood clots can also be categorized based on their movement—or whether or not they’re mobile. According to MedlinePlus, a blood clot that forms inside a vein or artery is called a thrombus (these can also form in your heart). But a blood clot that breaks free and moves from one part of the body is known as an embolus (or the plural form, emboli).
Arterial clots, aka arterial embolisms, when the clot or thrombus comes from elsewhere in the body—usually happens in the legs and feet, and interrupts blood flow to other parts of the body, according to the US National Library of Medicine’s MedlinePlus resource. Symptoms come on quickly or slowly, depending on the size of the clot and how much it blocks the flow of blood, but MedlinePlus states that you may not have any symptoms at all. An arterial clot that occurs in the brain can lead to a stroke, and one that forms in the heart can lead to a heart attack. But arterial clots can also show up in the kidneys, intestines, and even eyes—though those are rare.
A venous clot forms in a vein and can build up over time. According to the CDC, the most serious form of a venous clot is deep vein thrombosis (DVT), a condition that happens when a blood clot forms in a deep vein—as opposed to more superficial veins that are closer to the body’s surface. Those clots usually develop in the lower leg, thigh, or pelvis, but they can also occur in the arm. The most serious complication of DVT happens when a part of the clot breaks off and travels through the bloodstream to the lungs, the CDC explains. There, it can cause a blockage called pulmonary embolism (PE), stop blood from flowing to the lungs, and lead to death. DVTs, however, do not lead to heart attacks or stroke.
What To Do if You Have Symptoms
If you have any symptoms of a blood clot, seek medical attention ASAP. “You need to be seen,” Anita Gorwara, MD, family medicine physician and medical director of urgent care at Providence Saint John’s Health Center in Santa Monica, California, told Health. “Don’t waste time calling your doctor and waiting for them to get back to you. Go to an urgent care center, your primary care physician’s office, or the emergency room, right away.”
Timing matters with blood clots, because cells start dying after four minutes from lack of circulation. The experts say that this is why when someone has a stroke, the chance of damage to the brain can be minimized or eliminated if the clot is identified and treated promptly. To find out your risk level for having a blood clot or to check out the symptoms, you can also refer to the National Blood Clot Alliance website for more information. Dr. Levy stresses the importance of not brushing off your symptoms. “If you’re unsure, don’t assume it’s nothing,” he says. “Go get checked out.”
—
Photo Credit: studiovin / Shutterstock.com