So-called “good” HDL cholesterol may not be as healthy as experts once thought, a new study suggests.
As NBC News reports, the new study, published Wednesday in the medical journal Neurology, found that having either high or low levels of high-density lipoprotein, or HDL, cholesterol, may increase the risk of dementia in older adults. It’s more evidence showing that keeping HDL cholesterol within a certain range is important for cardiovascular and brain health.
“The relationship between HDL cholesterol and dementia is more complex than we previously thought,” said the study’s lead author, Erin Ferguson, a doctoral student studying epidemiology at the University of California San Francisco. “While the magnitude of this relationship is relatively small, it’s important,” The results show a correlation between HDL cholesterol and dementia, but do not prove that low or high levels of the lipid directly caused dementia.
The study, which was supported by the National Institute on Aging and the National Institutes of Health, included more than 184,000 adults with an average age of 70. None had dementia when the study began. Researchers used a combination of surveys and electronic records from the Kaiser Permanente Northern California health plan to track cholesterol levels, health behaviors and whether someone developed dementia over about 13 years. During that time, just more than 25,000 people developed dementia.
The study’s participants were divided into three groups based on their HDL cholesterol levels, with adjustments for other dementia risk factors, including high blood pressure, heart disease, diabetes and how often a person drinks.
What is a healthy level of HDL?
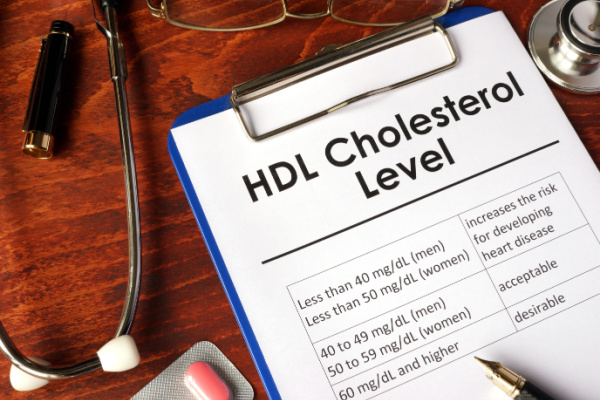
The Centers for Disease Control and Prevention recommends people keep their total cholesterol at about 150 mg/dL, or milligrams per deciliter of blood, with LDL at or below 100 mg/dL. Low-density lipoprotein, or LDL, cholesterol, has long been recognized for its often deadly impact on the cardiovascular system.
The average HDL cholesterol level in the study was 53.7 mg/dL, within the recommended range of 40 mg/dL in men and 50 mg/dL in women. People whose cholesterol levels strayed too far from these numbers were more likely to develop dementia over the course of the study. People whose levels were at least 65 mg/dL — the highest of the three groups — were 15% more likely to develop dementia. Those with the lowest levels — 11 to 41 mg/dL — had a 7% increased risk compared to the middle group.
The researchers didn’t find any association between LDL cholesterol and dementia risk.
Dr. Howard Weintraub, clinical director of the Center for the Prevention of Cardiovascular Disease at NYU Langone Heart in New York, said he was surprised by the findings. “When people have HDL that’s 90 or 100 mg/dL, that can be associated with increased cardiovascular risk, not necessarily dementia. These lower numbers, 53-63 mg/dL, have also not been associated with greater risk,” said Weintraub, who was not involved with the research.
Experts have long understood that not all HDL cholesterol is equal. How the body uses it and where it’s stored –– in the brain or elsewhere in the body –– make a difference.
How to improve HDL
Healthy habits, including exercise, allow HDL cholesterol to become HDL particles. This allows HDL to perform some of the important tasks it’s touted for, including removing LDL cholesterol from the arteries and transporting it to the liver, where the body gets rid of it, said Dr. Hussein Yassine, an endocrinologist at the Keck Medicine of USC who specializes in how changes in lipid metabolism impact a person’s risk of developing Alzheimer’s disease. “The function is really in the particles, not the cholesterol itself,” he said. “Simply increasing HDL levels does not increase its function.”
High HDL cholesterol levels can stiffen veins and arteries. This impact on the cardiovascular system is a key way high levels of HDL cholesterol may increase risk of cognitive impairment –– stroke is one of the leading risk factors for dementia. HDL cholesterol in the brain acts in a completely different way. “It operates on different rules and has different pathways than systemic cholesterol,” Yassine said. Systemic cholesterol is cholesterol stored elsewhere in the body, outside the brain.
Too much HDL cholesterol in the brain can cause inflammation that prompts the brain to produce amyloids, abnormal deposits that damage organs and tissues, he added.
Weintraub said there isn’t yet enough evidence to say that HDL cholesterol plays a significant role in dementia risk “This paper might suggest that HDL could be a modifiable risk factor even in late life,” Ferguson said. “But I wouldn’t say that people have to be worried about this just yet.”
Another recent study established a connection between genes linked to high HDL cholesterol levels and those that predispose someone to dementia. Together, the studies point to the fact that HDL cholesterol is both complex and an area of research that needs to be better understood.
—
Photo Credit: Vitalii Vodolazskyi / Shutterstock.com